Association between Oral Health Knowledge, Attitudes and Practices of Elderly Patients and chronic medical disorders in a Nigerian Tertiary Hospital
Keywords:
chronic diseases, elderly, Oral health perceptionAbstract
Background: Oral health of the elderly is an important component of general health and shares common risk factors. Poor oral health may signicantly inuence major chronic medical disorders, disability and quality of life in the elderly. The study sought to ascertain the knowledge of oral health and perceived impact of functional disability related systemic conditions among older adult patients.
Methods: A cross-sectional descriptive study was conducted on respondents aged 50 years and over attending General Practice Clinic, University of Benin Teaching Hospital, Benin City, Edo State, Nigeria, recruited by stratied sampling and surveyed using an interviewer-administered questionnaire.
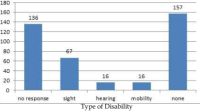
Results: A total of 392 respondents were included in the study period of which 157 (40.1%) were males and 235 (59.9%) females. The mean age of respondents was 61.9years (SD=6.8) Over half of the respondents (59%) had a chronic medical disorder with hypertension (31.4%) being the commonest. Also, disability (25.3%) was reported with visual impairment (17.1%) being the most common. Majority of the respondents (76.3%) had some knowledge of the dentist and dental caries (62.2%). On dental experiences (36.0%) had had tooth decay, gum bleeding (18.6%), dry mouth (45.2%), while with regards to practices they reported brushing daily (83.7%), previous dental visit (46%) and consumption of alcohol (18.4%). Furthermore 40.8%had knowledge that tobacco use could
predispose to halitosis, periodontal diseases (24.5%) cancer (40.8%) respectively. There was no significant relationship between chronic medical conditions and habits except in their knowledge of annual routine check-up.
Conclusions: The study demonstrated good oral health knowledge, attitudes and dental practices with low consumption of alcohol and tobacco among elderly patients. There is however for continuous health education, health promotion and surveillance. Dental professionals and policymakers need to pay greater attention to oral health associated chronic medical conditions.
Downloads
References
1. World Health Organization. Proposed working denition of an older person in Africa for the MDS project. 2016. Retrieved from http://www.who.int/healthinfo/survey/ageingdefnolder/en/
2. Abrams AP, Thompson LA. Physiology of ageing of older adults: systemic and Oral health considerations. Dent Clin North Am. 2014;58(4):729-38.
3. Petersen PE, Yamamoto T: Improving the oral health of older people: the approach of the WHO Global Oral Health Programme.
Community Dent Oral Epidemiol 2005; 33: 81–92.
4. Grifn SO, Jones JA, Brunson D, Grifn PM, Bailey WD. Burden of oral disease among older adults and implications for public health
priorities. Am J Public Health. 2012;102(3):411-8.
5. Paik Dl, Monn HS, Horowitz AM, Gitt HC, Jeong KL, Suh SS Knowledge of oral practices related to caries prevention among Koreans. J Public Health Dent 1994; 54:205-210
6. Gautam D K, Jindal V, Gupta S C, Tuli A, Kotwal B, Thakur R. Effect of cigarette smoking on the periodontal health status: A
comparative, cross sectional study. J Indian SocPeriodontol 2011;15:383-7
7. Genco RJ, Glurich I, Haraszthy V, Zambon J, DeNardin E Overview of Risk Factors for Periodontal Disease and Implications for Diabetes and Cardiovascular Disease. Compendium of Continuing Education in Dentistry 2001; 22(2):21-23
8. Alexander K, Raman P, Jennifer SW. Socioeconomic inequality in self-reported unmet need for oral health services in adults
aged 50 years and over in China, Ghana, and India Int J Equity Health. 2018; 17: 99.
9. Tran TD, Krausch-Hofmann S, Duyck J, de Almeida Mello J, De Lepeleire J. Association between oral health and general health indicators in older adults. Sci 2018,Rep 8:8871.
10. Khabra KK, Compton SM, Keenan LP. Independent older adults perspectives on oral health. Int J Dent Hyg 2017;15(4):295-305
11. Tavares M, LindefjeldCalabi KA, San Martin L. Systemic diseases and oral health. Dent Clin North Am 2014; 58:797-814.
12. Shimpi N, Jethwani M, Bharatkumar A, Chyou PH, Glurich I, Acharya A. Patient awareness/ knowledge toward oral cancer: a cross-
sectional survey. BMC Oral Health 2018;18:86.
13. Taiwo JO, Ibiyemi O, Bankole O. Oral Health Attitudes and Practices of the Elderly People in South-East Local Government Area
(SELGA) In Ibadan. Journal of Biology, Agriculture and Healthcare. 2012; 2(4): 53-58
14. Cochran, W.G. (1963) Sampling Techniques, Wiley, New York.
15. Saengtipbovorn S, Taneepanichskul S. Knowledge, attitude, and practice (KAP) toward oral health and diabetes mellitus among the elderly with type 2 diabetes, Bangkok, Thailand. J Health Res. 2014; 28(6): 433-41.
16.Walls AWG, Steele JG Geriatric oral health issues in the United Kingdom. International Dental Journal 2001; 51:183-187
17. Sheiham A, Steele J. Does the condition of the mouth and teeth affect the ability to eat certain foods, nutrient and dietary intake and nutritional status amongst older people? Public Health Nutrition 2001;4:797-803
18. Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, et al Hypertension Prevalence and Blood Pressure Levels in 6 European Countries, Canada, and the United States. JAMA. 2003;289(18):2363–2369.
19. Mahajan H, Kazi Y, Sharma B, Velhal GD. Assessment of KAP, risk factors and associated co-morbidities in hypertensive patients. IOSR J Dent Med Sci 2012; 1(2):6-14.
20. Al-Sharbatti S, Sadek M. Oral Health Knowledge, Attitudes and Practices of the elderly in Ajman, UAE. Gulf Med J 2014; 3(S2): S152-S64.
21. Spinler K, Aarabi G, Valdez R, Kofahl C, Heydecke G, König H et al. Prevalence and determinants of dental visits among older adults:
ndings of a nationally representative longitudinal study. BMC Health Serv Res. 2019; (19):590
22. Ehizele A O, Azodo C C, Ojehanon P I, Akhionbare O, Umoh A O, Adeghe H A. Prevalence of tobacco use among dental patients and their knowledge of its health effects. Niger J ClinPract 2012;15:270-5
23. Maxwell CJ, Hirdes JP. The prevalence of smoking and implications for quality of life among the community-based elderly. Am J
Prev Med 1993; 9:338-45.
24. Gupta R, Gupta S, Gupta P, Prakash H.Prevalence and determinants of hypertension in the urban population of Jaipur in western
India. J. Hypertens. 1995;13: 1193- 1200
25. Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L, et al. Socio- demographic patterning of non- communicable disease risk factors in rural India: A cross sectional study. BMJ 2010;341:c4974.
26. Nadkarni, A., Murthy, P., Crome, I. B., Rao, R. Alcohol use and alcohol- use disorders among older adults in India: a literature
review. Aging & Mental Health. 2013; 17(8):979–991. doi:10.1080/13607863.2013.793653
27. Lundgren, M., Osterberg, T., Emilson, G, Steen, B. Oral complaints and utilization of dental services in relation to general health factors
in a 88-year-old Swedish population. Gerodontology. 1995;12(2):81–88.
Downloads
Published
Issue
Section
License
All articles published in the journal are licensed under a Creative Commons Attribution (CC BY) license(i.e CC Attribution-NonCommercial-ShareAlike 4.0), allowing others to share, distribute, and build upon the work, provided the original author(s) and source are properly cited. Authors retain the copyright of their work.


