An Audit of Active Management of Third Stage of Labour in a Tertiary Hospital
Keywords:
postpartum haemorrhage, labour, third stage, Active managementAbstract
Background: Postpartum haemorrhage is a potentially life-threatening, but preventable condition which is the leading cause of maternal mortality globally. Active management of third stage of labour, has been found to be a useful intervention in the prevention of primary postpartum haemorrhage. However, the recent modication in the traditional Active management of third stage of labour by Royal College of Obstetricians and Gynaecologist, guideline would necessitate the auditing of our Active management of third stage of labour and postpartum haemorrhage in this centre.
Aim:To determine the effectiveness of Active management of third stage of labour in prevention of postpartum hemorrhage in Aminu Kano Teaching Hospital, Kano .
Methods: This is a two-year retrospective descriptive study done at Aminu Kano Teaching Hospital, Kano. Records of patients who delivered in this hospital, those that had AMTSL and those that had PPH were retrieved from the labour ward delivery record book. Patients' case les were retrieved, studied and recorded in a proforma. These were compared with the criteria obtained from the Royal College of Obstetricians and Gynaecologist guidelines. Data collected was fed into the computer and analyzed using SPSS Statistics version 19 software.
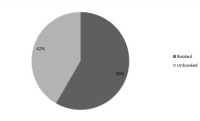
Results: During the study period, there were 4,827 clients that had vaginal delivery with active management of third stage of labour. One hundred and seven of them had postpartum hemorrhage, thus giving an incidence of 2.2%. Among the 107 cases, only 84 (78.5%) case notes could be retrieved from the medical records department and the labour ward register and these were the ones
analyzed. Twenty-three (21.5%) case note could not be retrieved. Among the 84 women whose case records were retrieved, the mean age of the subjects was 32 years S.D +/-1.3 years. The most common risk factor for Post-partum haemorrhage is Abruptio placentae
(53.3%). Administration of oxytocin and Controlled cord traction achieved standard for prevention of postpartum haemorrhage (95.2%).
Conclusion: This audit shows that Active management of third stage of labour by the use of oxytocics immediately after delivery and Controlled cord traction remain as effective as the recent World Health Organization revised Active Management of third stage of labour which involved use of oxytocics alone, in the prevention of postpartum haemorrhage.
Downloads
References
1. World Health Organization. WHO guidelines for the management of postpartum haemorrhage and retained placenta. Geneva: World Health Organization. 2009
2. Royal College of Obstetrician and Gynaecologists. Postpartum Hemorrhage: Prevention and Management. 2011.
3. World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. 2012. WHO: Geneva,
Switzerland
4. Gulmezoglu AM et al. Active management of the third stage of labour with and without controlled cord traction: a randomised, controlled,
noninferiority trial. Lancet 2012; March 6, 2012. DOI:10.1016/S0140-6736(12)60206-2
5. Zhu C, Estrada M, White J, Lal M. Heat- stable sublingual oxytocin tablets as a potential needle- free approach for preventing postpartum hemorrhage in low-resource settings. Drug Deliv Transl Res. 2018;8:853–6.
6. Oguz Orhan E, Dilbaz B, Aksakal SE, Altınbas S, Erkaya S. Prospective randomized trial of oxytocin administration for active management of the third stage of labor. Int J Gynecol Obstet. 2014;127:175–9.
7. Güngördük K, Asicioglu O, Celikkol O, Olgac Y, Ark C. Use of additional oxytocin to reduce blood loss at elective caesarean section: A randomised control trial. Austr N Z J Obstet Gynaecol. 2010;50:36–9.
8. Gohil JT, Tripathi B. A Study to Compare the Efcacy of Misoprostol, Oxytocin, Methyl- ergometrine and Ergometrine- Oxytocin in Reducing Blood Loss in Active Management of 3rd Stage of Labor. J Obstet Gynaecol India. 2011;61:408–12.
9. McDonald SJ, Abbott JM, Higgins SP. Prophylactic ergometrine-oxytocin versus oxytocin for the third stage of labour. Cochrane Database Syst Rev. 2004
10. 10. Mobeen N, Durocher J, Zuberi N, Jahan N, Blum J, Wasim S, et al. Administration of misoprostol by trained traditional birth
attendants to prevent postpartum haemorrhage in homebirths in Pakistan: a randomised placebo- controlled trial. BJOG. 2011;118:353–61.
11. Tuncalp Ö, Hofmeyr GJ, Gülmezoglu AM. Prostaglandins for preventing postpartum haemorrhage. Cochrane Database Syst Rev. 2012:CD000494.
12. Tan J, Cao Q, He GL, Cai YH, Yu JJ, Sun X, et al. Misoprostol versus ergometrine-oxytocin for preventing postpartum haemorrhage: a systematic review and meta-analysis of randomized controlled trials. J Evid Based Med. 2016;9:194–204.
13. Hernández-Castro F, López-Serna N, Treviño-Salinas EM, Soria- López JA, Sordia-Hernández LH, Cárdenas-Estrada E. Randomized double-blind placebo-controlled trial of buccal misoprostol to reduce the need for additional uterotonic drugs during cesarean delivery. Int J Gynaecol Obstet. 2016;132:184–7.
14. Wishart DS, Feunang YD, Guo AC, Lo EJ, Marcu A, Grant JR, et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res.2018;46(D1):D1074–82. doi:10.1093/nar/gkx1037.
15. Kim S, Thiessen PA, Bolton EE, Chen J, Fu G, Gindulyte A, et al. PubChem Substance and Compound databases. Nucleic Acids Res. 2016 ;44 (D1): D1202 – 13. doi:10.1093/nar/gkv951.
16. The international pharmacopoeia, seventh edition. Geneva: World Health Organization;2017.
17. Hofmeyr GJ, Mshweshwe NT, Gülmezoglu AM. Controlled cord traction for the third stage of labour. Cochrane Database Syst Rev. 2015;1:CD008020.
18. Gungorduk K, Yıldırım G, Asıcıoğlu O, Gungorduk OC, Sudolmus S, Ark C. Efcacy of intravenous tranexamic acid in reducing
blood loss after elective cesarean section: a prospective, randomized, double-blind, placebo- controlled study. Am J Perinatol. 2011;28:233–40.
19. Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database of Syst Rev. 2015:CD007412.
20. MillerS, Lester F, Hensleigh P. Prevention and treatment of Postpartum Haemorrhage: new advances for low-resource settings. J Midwifery Womens Health. 2004; 49 (4): 283-92.
21. Garba Z, Musa H, Yusuf M,Usman I,Danladi I, appropriate documentation of the timing of events in the management of PPH in AKTH. NigerMed J 2019; 60:9-12.
22. Mutihir JT, Utoo B T. Postpartum maternal morbidity in Jos, North-Central Nigeria. Niger J Clin Pract 2011; 14:38-42
23. AS Adeniran, MA Ijaiya, AP Aboyeji, OR Balogun, AA Fawole, KT Adesina j Primary Postpartum Haemorrhage [PPH] In Ilorin: Current Trends j of African health 2014;21;2.
24. Kinikanwo I G, John D O, Mmom C F. Primary Postpartum Haemorrhage at the University of Port Harcourt Teaching Hospital: Prevalence and Risk Factors. The Nigerian Health Journal, 2015;15:23-5
25. B-Lynch C, Keith LG, Lalonde AB, Karoshi M (eds). A Textbook of Postpartum Haemorrhage: a comprehensive guide to evaluation, management and surgical intervention. Kirkmahoe, UK: Sapiens Publishing, 2006:123-126.
26. Oyelese Y, Anath CV. Postpatum heamorrhage: epidemiology, risk factors and causes. Clin Obstet Gynecol. 2010; 53(1): 147- 56 20.
27. WHO recommendations Uterotonics for the prevention of postpartum haemorrhage, 2018.
Downloads
Published
Issue
Section
License
All articles published in the journal are licensed under a Creative Commons Attribution (CC BY) license(i.e CC Attribution-NonCommercial-ShareAlike 4.0), allowing others to share, distribute, and build upon the work, provided the original author(s) and source are properly cited. Authors retain the copyright of their work.


